Cancer of the womb (uterus) is a common cancer of the female reproductive system that often causes abnormal vaginal bleeding.
OVERVIEW
CANCER OF THE WOMB (UTERINE OR ENDOMETRIAL CANCER) IS A COMMON CANCER THAT AFFECTS THE FEMALE REPRODUCTIVE SYSTEM. IT’S MORE COMMON IN WOMEN WHO HAVE BEEN THROUGH THE MENOPAUSE.
SYMPTOMS OF WOMB CANCER
The most common symptom of womb cancer is vaginal bleeding that is unusual for you (abnormal). If you’ve been through the menopause, any vaginal bleeding is considered abnormal. If you have not yet been through the menopause, abnormal bleeding may include very heavy periods or bleeding between your periods. Read more about the symptoms of womb cancer.
CORONAVIRUS ADVICE
Get advice about coronavirus and cancer:
- Macmillan: Coronavirus guidance for people with cancer
- Cancer Research UK: Coronavirus and cancer
WHEN TO SEE A GP
See your GP as soon as possible if you experience any unusual vaginal bleeding. While it’s unlikely to be caused by womb cancer, it’s best to be sure. Your GP will ask about your symptoms and offer an internal examination. They will refer you to a specialist if necessary for further tests to rule out any serious problem.
TYPES OF WOMB CANCER
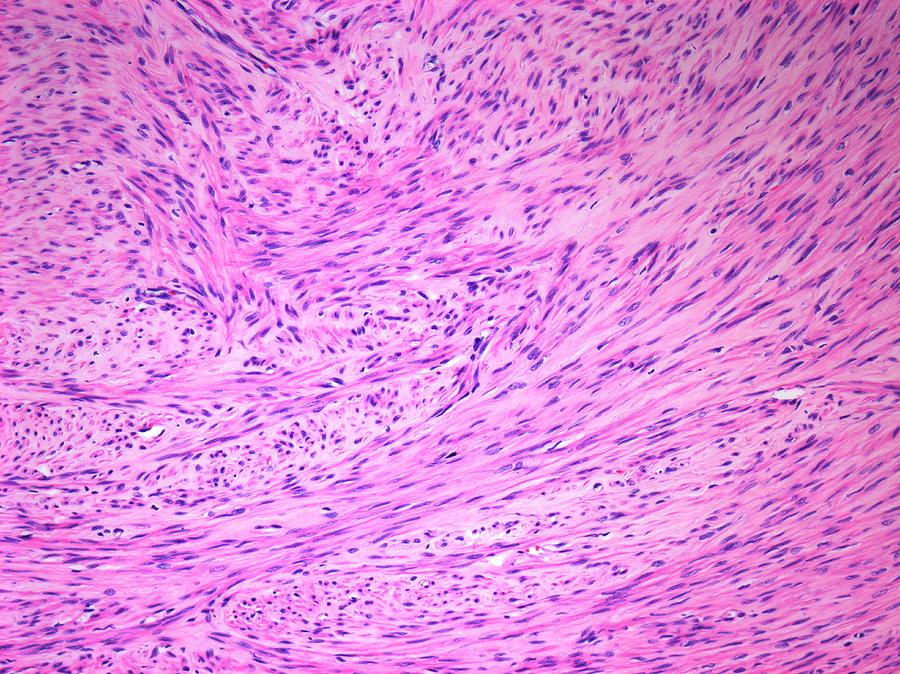
Most womb cancers begin in the cells that make up the lining of the womb (the endometrium). This is why cancer of the womb is often called endometrial cancer. In rare cases, womb cancer can start in the muscle wall of the womb. This type of cancer is called uterine sarcoma and may be treated in a different way. Read more about soft tissue sarcomas. Womb cancer is separate from other cancers of the female reproductive system, such as ovarian cancer and cervical cancer.
WHY DOES WOMB CANCER HAPPEN?
It’s not clear exactly what causes womb cancer, but certain things can increase your risk of developing it. One of the main risk factors for womb cancer is higher levels of a hormone called oestrogen in your body. A number of things can cause your oestrogen levels to be high, including obesity. There is also a small increase in the risk of womb cancer with long-term use of the breast cancer drug tamoxifen. It’s not always possible to prevent womb cancer, but some things are thought to reduce your risk. This includes maintaining a healthy weight and the long-term use of some types of contraception.
TREATING WOMB CANCER
The most common treatment for womb cancer is the surgical removal of the womb (hysterectomy). A hysterectomy can cure womb cancer in its early stages, but you will no longer be able to get pregnant. Surgery for womb cancer is also likely to include the removal of the ovaries and fallopian tubes. Radiotherapy or chemotherapy are also sometimes given too. A type of hormone therapy (progestogen) may be used if you have not yet been through the menopause and would still like to have children. Even if your cancer is advanced and the chances of a cure are small, treatment can still help to relieve symptoms and prolong your life.
LIVING WITH WOMB CANCER
Living with cancer is challenging, and womb cancer can affect your life in specific ways. For example, your sex life may be affected if you have a hysterectomy, especially if your ovaries are removed. You may find it physically more difficult to have sex and also have a reduced sex drive. You may find it beneficial to talk to other people about your condition, including family members, your partner or other people with womb cancer.
SYMPTOMS
THE MOST COMMON SYMPTOM OF WOMB CANCER IS UNUSUAL (ABNORMAL) BLEEDING FROM THE VAGINA, ALTHOUGH MOST PEOPLE WITH ABNORMAL BLEEDING DO NOT HAVE CANCER.
It may start as light bleeding and a watery discharge, which may get heavier over time. Most women diagnosed with womb cancer have been through the menopause, so any vaginal bleeding will be unusual. In women who have not been through the menopause, unusual vaginal bleeding may be:
- periods that are heavier than usual
- vaginal bleeding in between normal periods
Less common symptoms include pain in the lower abdomen (tummy) and pain during sex. If womb cancer reaches a more advanced stage, it may cause additional symptoms. These include:
- pain in the back, legs or pelvis
- loss of appetite
- tiredness
- nausea
WHEN TO SEE A GP
See a GP if you have bleeding after the menopause or notice a change in the normal pattern of your period. Only 1 in 10 cases of vaginal bleeding after the menopause are caused by womb cancer, so it’s unlikely your symptoms will be caused by this. However, if you have unusual vaginal bleeding, it’s important to investigate the cause. The bleeding may be the result of a number of other potentially serious health conditions, such as:
- endometriosis – where tissue that behaves like the lining of the womb is found outside of the womb
- tside of the womb
Other types of gynaecological cancers can also cause unusual vaginal bleeding, particularly cervical cancer.
CAUSES
IT’S NOT KNOWN EXACTLY WHAT CAUSES WOMB CANCER, ALTHOUGH A NUMBER OF THINGS CAN INCREASE YOUR RISK OF DEVELOPING THE CONDITION.
AGE
The risk of womb cancer increases with age. Most cases occur in women aged 40 to 74, with only 1% of cases being diagnosed in women under 40.
OESTROGEN LEVELS AFTER THE MENOPAUSE
The risk of developing womb cancer is linked to the body’s exposure to oestrogen. Oestrogen is one of the hormones that regulates the reproductive system in women:
- oestrogen stimulates the release of eggs from your ovaries and causes the cells of the womb lining to divide
- progesterone gets the lining of your uterus ready to receive the egg from the ovaries
The levels of oestrogen and progesterone in your body are usually balanced. If oestrogen is not kept in check by progesterone, it can increase. This is called unopposed oestrogen. After the menopause, the body stops producing progesterone. However, there are still small amounts of oestrogen being produced. This unopposed oestrogen causes the cells of the endometrium to divide, which can increase the risk of womb cancer.
BEING OVERWEIGHT OR OBESE
As oestrogen can be produced in fatty tissue, being overweight or obese increases the level of oestrogen in your body. This significantly increases your chances of developing womb cancer. Women who are overweight are 3 times more likely to develop womb cancer compared with women who are a healthy weight. Very obese women are 6 times more likely to develop womb cancer compared with women who are a healthy weight. One way to assess if you are a healthy weight is to calculate your body mass index (BMI).
REPRODUCTIVE HISTORY
Women who have not had children are at a higher risk of womb cancer. This may be because the higher levels of progesterone and lower levels of oestrogen that occur during pregnancy have a protective effect on the lining of the womb.
TAMOXIFEN
Women who take tamoxifen – a hormone treatment for breast cancer – can be at an increased risk of developing womb cancer. However, this risk is outweighed by the benefits that tamoxifen provides in preventing breast cancer. It’s important to visit your GP if you’re taking tamoxifen and experience any abnormal vaginal bleeding.
HIGH LEVELS OF INSULIN
Conditions such as hyperinsulinaemia, where your body produces more insulin than normal, can increase the risk of tumours.
POLYCYSTIC OVARY SYNDROME (PCOS)
Women with polycystic ovary syndrome (PCOS) are at a higher risk of developing womb cancer, as they have high levels of oestrogen in their bodies. Women with PCOS have lots of cysts in their ovaries, which can cause symptoms such as irregular or light periods, or no periods at all, as well as problems getting pregnant, weight gain, acne and excessive hair growth (hirsutism).
ENDOMETRIAL HYPERPLASIA
Endometrial hyperplasia is when the lining of the womb becomes abnormally thicker. Women with the condition may be at an increased risk of developing womb cancer.
DIAGNOSIS
SEE A GP IF YOU HAVE ABNORMAL VAGINAL BLEEDING. WHILE IT’S UNLIKELY TO BE CAUSED BY WOMB CANCER, IT’S BEST TO BE SURE.
Your GP will ask about your symptoms, and when and how often they happen. You will be offered a physical (internal) examination to assess your pelvic organs, including your womb and ovaries.
TRANSVAGINAL ULTRASOUND SCAN (TVS)
A TVS is a type of ultrasound scan that uses a small probe as a scanner. This is placed directly into the vagina to get a detailed picture of the inside of the womb. The probe can feel a little uncomfortable but should not be painful. The TVS checks whether there are any changes to the thickness of the lining of your womb that could have been caused by the presence of a polyp or cancerous cells.
HYSTEROSCOPY AND BIOPSY
If the TVS detects changes in the thickness of the lining of your womb, you’ll usually be offered a hysteroscopy. This is where a thin type of telescope (hysteroscope) is inserted through your vagina and into your womb, allowing a healthcare professional to look at the lining of the womb. You are likely to have a biopsy at the same time. This involves taking a sample from the lining of your womb (the endometrium). The sample is then checked for cancerous cells at a laboratory. This is usually an outpatient procedure where you will not need to stay in hospital. Sometimes you may have a biopsy without hysteroscopy, called “aspiration biopsy”. This is where a small flexible tube, inserted into your vagina and up into your womb, is used to suck up a small sample of cells. In some cases, a hysteroscopy and dilatation and curettage (D&C) may be offered. D&C is a minor surgical procedure carried out under general anaesthetic (while you’re asleep), where some tissue from the womb lining (biopsy) is removed. The tissue is then sent off to a laboratory for further testing.
FURTHER TESTS IF YOU HAVE WOMB CANCER
If you’re diagnosed with womb cancer, you may have further tests to help determine what stage it is. Staging allows the doctors to work out how large the cancer is, whether it has spread and the best treatment options for you. These tests may include:
- a chest X-ray – where radiation is used to check if the cancer has spread to your lungs
- an MRI scan – where magnetic fields are used to create a detailed image of the inside of your body to check if the cancer has spread
- a CT scan – where a series of X-rays are used to create a detailed image of the inside of your body to check if the cancer has spread
- further blood tests – these are usually done to check your general health and how well some of your organs are functioning
The levels of oestrogen and progesterone in your body are usually balanced. If oestrogen is not kept in check by progesterone, it can increase. This is called unopposed oestrogen. After the menopause, the body stops producing progesterone. However, there are still small amounts of oestrogen being produced. This unopposed oestrogen causes the cells of the endometrium to divide, which can increase the risk of womb cancer.
BEING OVERWEIGHT OR OBESE
As oestrogen can be produced in fatty tissue, being overweight or obese increases the level of oestrogen in your body. This significantly increases your chances of developing womb cancer. Women who are overweight are 3 times more likely to develop womb cancer compared with women who are a healthy weight. Very obese women are 6 times more likely to develop womb cancer compared with women who are a healthy weight. One way to assess if you are a healthy weight is to calculate your body mass index (BMI).
REPRODUCTIVE HISTORY
Women who have not had children are at a higher risk of womb cancer. This may be because the higher levels of progesterone and lower levels of oestrogen that occur during pregnancy have a protective effect on the lining of the womb.
TAMOXIFEN
Women who take tamoxifen – a hormone treatment for breast cancer – can be at an increased risk of developing womb cancer. However, this risk is outweighed by the benefits that tamoxifen provides in preventing breast cancer. It’s important to visit your GP if you’re taking tamoxifen and experience any abnormal vaginal bleeding.
HIGH LEVELS OF INSULIN
Conditions such as hyperinsulinaemia, where your body produces more insulin than normal, can increase the risk of tumours.
POLYCYSTIC OVARY SYNDROME (PCOS)
Women with polycystic ovary syndrome (PCOS) are at a higher risk of developing womb cancer, as they have high levels of oestrogen in their bodies. Women with PCOS have lots of cysts in their ovaries, which can cause symptoms such as irregular or light periods, or no periods at all, as well as problems getting pregnant, weight gain, acne and excessive hair growth (hirsutism).
ENDOMETRIAL HYPERPLASIA
Endometrial hyperplasia is when the lining of the womb becomes abnormally thicker. Women with the condition may be at an increased risk of developing womb cancer.
TREATMENT
SURGERY IS OFTEN THE MAIN TREATMENT FOR WOMB CANCER. THE BEST TREATMENT WILL DEPEND ON YOUR INDIVIDUAL CIRCUMSTANCES.
YOUR CANCER CARE TEAM
People with cancer should be cared for by a team of specialists.
The team often consists of a specialist cancer surgeon, an oncologist (a radiotherapy and chemotherapy specialist), a radiologist, a pathologist, a radiographer and a specialist nurse.
Other members may include a dietitian, a physiotherapist and an occupational therapist. You may also have access to clinical psychology support.
When deciding which treatment is best for you, your healthcare professionals will consider:
-
- the type and size of the cancer
- what grade it is
- your general health
- whether the cancer has spread to other parts of your body
‘
- whether fertility is a matter of concern – this is rare because of the age that womb cancer usually occurs
They will discuss and recommend the best treatment for you based on these considerations. The final decision on which type of treatment you have, if any, is always yours.
Before going to hospital to discuss your treatment options, it can be useful to write a list of questions you would like to ask the specialist. For example, you may want to find out what the advantages and disadvantages of particular treatments are.
The stages of womb cancer and the main treatment options are outlined below.
STAGES OF WOMB CANCER
Doctors will use the results of your tests to identify the “stage” of your cancer (how far the cancer has spread). The stage will determine which types of treatments will be necessary.
Your chances of surviving womb cancer depend on the stage at which it’s diagnosed.
TREATMENT OVERVIEW
The main treatment for womb cancer is to remove the womb (hysterectomy) together with the ovaries and fallopian tubes.
This is sometimes followed by radiotherapy or chemotherapy to try to kill any possible remaining cancer cells, depending on the stage and grade of the cancer.
TREATMENT FOR WOMEN WHO HAVE NOT BEEN THROUGH THE MENOPAUSE
Advanced womb cancer requires a different course of treatment, usually depending more on chemotherapy.
Advanced cancer may not be curable, but the treatment aims to achieve a remission, where the cancer shrinks, making you feel normal and able to enjoy life to the full.
Even if there’s no chance of a cure, surgery may be carried out to remove as much of the cancer as possible.
Radiotherapy, chemotherapy or hormone therapy can reduce symptoms such as pain by shrinking the cancer or slowing its growth.
SURGERY
SURGERY FOR STAGE 1 WOMB CANCER
If you have stage 1 cancer, you’ll probably have a hysterectomy. This involves removing the womb, as well as both ovaries and the fallopian tubes, in a procedure called a bilateral salpingo-oophorectomy (BSO).
The surgeon may also take samples from the lymph nodes in the pelvis and abdomen, and other nearby tissue. These will be sent to the laboratory to see whether the cancer has spread.
Hysterectomy may be performed as keyhole surgery using a telescope (laparoscopic hysterectomy) or with a large cut across your tummy (abdominal hysterectomy). Laparoscopic hysterectomy has the benefit of minimal scarring and quicker recovery.
You’ll probably be ready to go home 1 to 3 days after your operation, depending on the type of surgery. But it can take many weeks to recover fully.
After your operation, you’ll be encouraged to start moving about as soon as possible. This is very important.
Even if you have to stay in bed, you’ll need to keep doing regular leg movements to help your circulation and prevent blood clots. You’ll be shown exercises by the nurses or physiotherapist to help prevent complications.
When you go home, you’ll need to exercise gently to build up your strength and fitness. Discuss with your doctor or physiotherapist which types of exercise would be suitable for you.
SURGERY FOR STAGE 2 OR 3 WOMB CANCER
f you have stage 2 or 3 womb cancer and the cancer has spread to the cervix or nearby lymph nodes in the pelvis, you may have a radical or total hysterectomy.
This involves the additional removal of the cervix and the top of your vagina, as well as the removal of the pelvic lymph nodes. You may also need radiotherapy or chemotherapy after surgery to reduce the risk of the cancer returning.
SURGERY FOR ADVANCED CANCER (STAGE 4)
If you have advanced womb cancer, you may have surgery to remove as much of the cancer as possible. This is called debulking surgery.
This won’t cure the cancer, but it may ease some of the symptoms. Your doctor will discuss whether debulking surgery is suitable for you.
RADIOTHERAPY
A course of radiotherapy will be recommended if your treatment team thinks there’s a significant risk the cancer could return in the pelvis.
Radiotherapy may also be used to slow the spread of cancer when a surgical cure is not possible.
There are two types of radiotherapy used to treat womb cancer:
- internal radiotherapy (also called brachytherapy) – where a plastic tube is inserted inside the womb and radiation treatment is passed down the tube into the womb
- external radiotherapy – where a machine is used to deliver pulses of radiation to your pelvis
A course of external radiotherapy is usually given to you as an outpatient for 5 days a week, with a break at the weekend. The treatment takes a few minutes. The whole course of radiotherapy may last approximately 4 weeks, depending on the stage and position of the womb cancer.
Some women have brachytherapy as well as external radiotherapy. During brachytherapy, the device that delivers radiation is placed in your vagina.
There are different types of brachytherapy, involving either low, medium or high dose rates. With low-dose-rate methods, the radiation is delivered more slowly, so the device has to stay inside you for longer. You’ll have to stay in hospital while you have the treatment. Your doctor will discuss this with you.
Radiotherapy has some side effects. Skin in the treated area can become red and sore, and hair loss may occur. Radiotherapy to the pelvic area can affect the bowel and cause sickness and diarrhoea.
As your course of treatment progresses, you’re likely to get very tired. Most of these side effects will go away when your treatment finishes, although around 5% of women experience long-term treatment effects, such as diarrhoea and bleeding from the bottom.
CHEMOTHERAPY
If you have stage 3 or 4 womb cancer, you may be given a course of chemotherapy.
Chemotherapy can be used after surgery to try to prevent the return of the cancer. In cases of advanced cancer, it may be used to slow the spread of the cancer and relieve symptoms.
Chemotherapy is usually given as an injection into the vein (intravenously). You’ll usually be able to go home the same day you have chemotherapy, but sometimes you may need a short stay in hospital.
Chemotherapy is usually given in cycles, with a period of treatment followed by a period of rest to allow the body to recover.
- nausea
- vomiting
- hair loss
- fatigue
There is also an increased risk of an infection developing in your bloodstream (sepsis), as your body’s ability to fight infection is reduced by chemotherapy.
The side effects should stop once treatment has finished.
HORMONE THERAPY
Some womb cancers are affected by the female hormone oestrogen. These cancers may respond to treatment with hormone therapy. Your doctor will discuss whether this is a possible treatment for your womb cancer.
Hormone therapy usually replaces a hormone called progesterone, which occurs naturally in your body. It uses artificial progesterone and is usually given as tablets.
The treatment is mainly used for advanced-stage womb cancers or cancer that has come back, and can help shrink the tumour and control any symptoms.
The treatment may have some side effects, including mild nausea, mild muscle cramps and weight gain. Your doctor will discuss these with you.
CLINICAL TRIALS
A lot of progress has been made in the treatment of womb cancer, and more women are living longer with fewer side effects. Some of these advances came through clinical trials, where new treatments and combinations of treatments are compared with standard treatment.
All cancer clinical trials in the UK are carefully monitored to make sure the trial is worthwhile and safely conducted. Participants in clinical trials often do better overall than those in routine care.
If you’re invited to take part in a trial, you’ll be given an information sheet. If you wish to take part, you’ll be asked to give consent. You’re always free to refuse or withdraw from a clinical trial without it affecting your care
LIVING WITH
A CANCER DIAGNOSIS IS A CHALLENGE FOR MOST PEOPLE. HOW CANCER AFFECTS YOUR DAILY LIFE DEPENDS ON THE STAGE OF YOUR CANCER AND THE TREATMENTS USED.
There are many ways to get help coping with cancer. They do not all work for everybody, but one or more should prove helpful:
- keep talking to your friends and family – they can be a powerful support system
- communicate with others in the same situation
- learn about your condition
- set reasonable goals
- take time out for yourself
AFTER TREATMENT
Women with womb cancer usually have a hysterectomy. This can be a major operation, and recovery may take from 6 to 12 weeks. During this time, you will have to avoid lifting things – for example, children and heavy shopping bags – and doing heavy housework. You will not be able to drive for between 3 and 8 weeks after the operation. Most women need 4 to 12 weeks off work after a hysterectomy. The recovery time will depend on the type of surgery you have, whether or not any problems develop and what type of work you will return to. Some of the treatments for endometrial cancer, particularly radiotherapy, can make you very tired. You may need to take a break from some of your normal activities for a while. Don’t be afraid to ask for practical help from family and friends if you need it.
FOLLOW-UP
After your course of treatment has finished, you’ll probably be invited back for regular check-ups. At the check-up, your doctor will examine you – this is likely to include an internal examination – and possibly carry out blood tests or scans to see how your cancer is responding to treatment Advanced cancer may not be curable, but the treatment aims to achieve a remission, where the cancer shrinks, making you feel normal and able to enjoy life to the full.
RELATIONSHIPS AND SEX
Knowing how to talk to your friends and family about your cancer can be difficult, and they may find it hard to talk to you, too. People deal with serious problems in different ways. It’s hard to predict how a diagnosis of cancer will affect you. Being open and honest about how you feel and what your family and friends can do to help may put them at ease. But don’t feel shy about telling people that you want some time to yourself, if that’s what you need. YOUR SEX LIFE Womb cancer and its treatment can affect your sex life. This can happen in several ways. If you haven’t already had the menopause, removing the ovaries means you’ll go through an early menopause. Symptoms can include vaginal dryness and loss of sexual desire. Radiotherapy for endometrial cancer can make your vagina narrower and less flexible. Sometimes, the vagina gets so narrow having sex becomes difficult. To stop this happening, you should be offered a set of vaginal dilators, which are plastic cones you put into your vagina to stretch it. You can also stretch your vagina by having sex, or by using your fingers or a vibrator. It’s common for women to lose interest in sex after treatment for womb cancer. Your treatment may leave you feeling very tired. You may feel shocked, confused or depressed about being diagnosed with cancer, and you also may be grieving the loss of your fertility. It’s understandable that you may not feel like having sex while having to cope with all this. Try to share your feelings with your partner. If you feel you have problems with sex that are not getting better with time, you may want to speak to a counsellor or sex therapist.
TALKING TO OTHERS
Being diagnosed with cancer can be hard for patients and their families. You’ll need to deal with the emotional and practical difficulties. With womb cancer, you have to cope physically with recovering from a hysterectomy as well as the possible emotional impact of losing your womb. Younger women may have to face the fact they won’t be able to have children, and cope with the grief and anger that may cause. It can often help to discuss your feelings and other difficulties with a trained counsellor or therapist. You can ask for this kind of help at any stage of your illness. There are various ways to find help and support:
- if you’re struggling with feelings of depression, talk to your GP – a course of antidepressant drugs may be helpful, or your GP can refer you to a counsellor or psychotherapist
- many organisations have telephone helplines and forums, and can put you in touch with other people who have been through cancer treatment
MONEY AND FINANCIAL SUPPORT
If you have to limit or stop work because of your cancer, you may find it hard to cope financially. If you have cancer or are caring for someone with cancer, you may be entitled to financial support.
- if you have a job but cannot work because of your illness, you’re entitled to Statutory Sick Pay from your employer
- if you do not have a job and cannot work because of your illness, you may be entitled to Employment and Support Allowance
- if you’re caring for someone with cancer, you may be entitled to Carer’s Allowance
- you may be eligible for other benefits if you have children living at home or you have a low household income
Find out early on what help is available to you. You can ask to speak to the social worker at your hospital, who can give you the information you need.
FREE PRESCRIPTIONS
People being treated for cancer are entitled to apply for a certificate giving free prescriptions for all medication, including medicine for unrelated conditions. The certificate is valid for 5 years, after which you can apply for it to be renewed. You can apply for a certificate by speaking to your GP or cancer specialist.
DEALING WITH DYING
If you’re told nothing more can be done to treat your womb cancer, your care will focus on controlling your symptoms and helping you to be as comfortable as possible. This is called palliative care. Palliative care also includes psychological, social and spiritual support for you and your family or carers.