The removal of wisdom teeth, or third molars, is one of the most common procedures carried out in the UK.
OVERVIEW
Your wisdom teeth don’t usually need to be removed if they’re impacted but aren’t causing any problems. This is because there’s no proven benefit of doing this and it carries the risk of complications. Sometimes, wisdom teeth that have become impacted or haven’t fully broken through the surface of the gum can cause dental problems. Food and bacteria can get trapped around the edge of the wisdom teeth, causing a build-up of plaque, which can lead to:
- tooth decay (dental caries)
- gum disease (also called gingivitis or periodontal disease)
- pericoronitis – when plaque causes an infection of the soft tissue that surrounds the tooth
- cellulitis – a bacterial infection in the cheek, tongue or throat
- abscess – a collection of pus in your wisdom teeth or the surrounding tissue as a result of a bacterial infection
- cysts and benign growths – very rarely, a wisdom tooth that hasn’t cut through the gum develops a cyst (a fluid-filled swelling)
Many of these problems can be treated with antibiotics and antiseptic mouthwash. Wisdom teeth removal is usually recommended when other treatments haven’t worked.
HOW IT’S PERFORMED
ANAESTHESIA
Before having your wisdom teeth removed, you’ll be given an injection of local anaesthetic to numb the tooth and surrounding area. If you’re particularly anxious about the procedure, your dentist or surgeon may give you a sedative to help you relax. This will usually be an injection into your arm. General anaesthetic is rarely needed for wisdom tooth removal. It’s only occasionally used when the procedure is carried out in hospital. However, in this case, you should still be able to go home on the same day as the procedure.
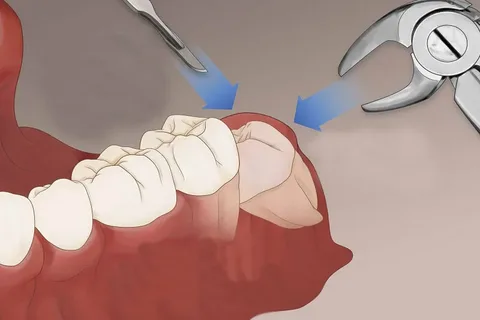
REMOVING THE WISDOM TOOTH
If the tooth hasn’t come through the gum, a small cut (incision) will be made in the gum to access it. A small piece of the bone covering the tooth may also need to be removed. The tooth may be cut into smaller parts to make it easier to remove through the opening. There’s less need to make an incision if the tooth has broken through the gum. You’ll feel some pressure just before the tooth is removed, as your dentist or oral surgeon needs to widen the tooth socket by rocking the tooth back and forth before taking it out. You shouldn’t feel any pain as your wisdom teeth are removed because the area will be numb. However, if you do feel pain during the procedure, tell your dentist or oral surgeon so they can give you more anaesthetic. How long it takes to remove the tooth will vary. Simple procedures can take a few minutes, but it can take longer than 20 minutes if it’s more complicated.
AFTER SURGERY
If an incision has been made, dissolving stitches are used to seal the gum. Your dentist will tell you how long the stitches take to dissolve (usually 7 to 10 days). Your dentist may place gauze over the site of the extraction and ask you to keep pressure on it by biting your jaws together for up to an hour. This is to allow a blood clot to form in the empty tooth socket. Blood clots are part of the healing process, so try not to dislodge them. In some cases, antibiotics may be prescribed if you have an ongoing infection. For the 24 hours after removing your wisdom tooth, you should avoid:
- rinsing your mouth out with liquid
- drinking alcohol and smoking
- drinking hot liquids such as tea or soup
- strenuous physical activity
RECOVERY
It can take up to 2 weeks to fully recover after having your wisdom teeth removed. During this time, you may have:
- a swollen mouth and cheeks – this will be worse for the first few days but will gradually improve; gently pressing a cold cloth to your face helps reduce the swelling
- some mild visible bruising of your cheek – the skin may be bruised for up to 2 weeks
- a stiff, sore jaw – this should wear off within 7 to 10 days
- pain – this is worse if the extraction was difficult or complicated
- an unpleasant taste in your mouth
- tingling or numbness of your face, lips or tongue (although this is uncommon)
Report any excess bleeding, severe pain or any other unusual symptoms to your dentist or oral surgeon immediately.
SELF-CARE ADVICE
To reduce pain and aid your recovery, it can be helpful to:
- use painkillers such as paracetamol or ibuprofen (always read and follow the manufacturer’s dosage instructions) – there’s some evidence to suggest that ibuprofen is the best painkiller to take after having wisdom teeth removed
- avoid strenuous activity and exercise for a few days
- use an extra pillow to support your head at night
- for 24 hours, avoid rinsing, spitting, hot drinks or anything else that may dislodge the blood clots that form in the empty tooth socket (they help the healing process)
- avoid smoking and drinking alcohol for 24 hours
- eat soft or liquid food for a few days and chew with your other teeth
- gently rinse the extraction site with antiseptic mouthwash after 24 hours, and repeat this regularly over the next few days, particularly after eating – you can also use warm water with a teaspoon of salt as mouthwash to reduce gum soreness and inflammation
WORKING AND DRIVING
It’s usually recommended that you take a day or two off work after having a wisdom tooth removed. You won’t need a sick note from your doctor or dentist for this. You can drive immediately after the procedure if local anaesthetic was used, but you should avoid driving for at least 24 hours if a sedative was used, or 48 hours if the procedure was carried out under general anaesthetic.
RETURNING TO NORMAL
After your wisdom teeth have been removed and any swelling and bruising has disappeared, your mouth and face should return to normal. You’ll usually be able to brush your teeth normally after a few days. Make sure you finish any course of antibiotics you’ve been given. A check-up appointment may be arranged for about a week or so after the procedure. At this point, any remaining stitches may be removed.
COMPLICATIONS
As with any type of surgery, wisdom tooth removal carries some risks. However, these risks are usually small. Risks can include:
- dry socket – where a blood clot fails to develop in the tooth socket, or if the blood clot becomes dislodged
- nerve injury – this can cause temporary or permanent problems, such as tingling or numbness
- infection – signs include a high temperature, yellow or white discharge from the extraction site, and persistent pain and swelling
- bleeding
See your dentist if you have signs of infection after having your wisdom teeth removed, or if you’re bleeding heavily from the extraction site.
DRY SOCKET
Dry socket (alveolar osteitis) is one of the most common complications of wisdom tooth removal. It’s where a blood clot fails to develop in the tooth socket, or if the blood clot becomes dislodged or disappears. This can happen 3 to 5 days after surgery. The empty socket causes an ache or throbbing pain in your gum or jaw, which can be intense like a toothache. There may also be an unpleasant smell or taste from the empty tooth socket. If you look into the socket, you might be able to see exposed bone rather than a blood clot. You’re more at risk of developing dry socket if:
- you don’t follow your dentist’s instructions after the extraction
- you smoke
- you’ve had the condition before
- you’re over 25 years old
- the extraction was difficult or complicated
See your dentist or surgeon if you think you have dry socket. They can flush any debris out of the socket or cover it with a medicated dressing, which may be removed and replaced frequently until it heals.
NERVE INJURY
Although far less common than dry socket, injury to sections of a nerve called the trigeminal nerve is another possible complication of wisdom tooth removal. It can cause pain, a tingling sensation and numbness in your tongue, lower lip, chin, teeth and gums. The damage is usually temporary, lasting for a few weeks or months. However, it can be permanent if the nerve has been severely damaged. A nerve injury can interfere with your daily activities, making things such as eating and drinking difficult. However, a nerve injury will only cause sensation problems – it won’t cause any weakness to your lip or tongue. Your dentist or surgeon will try to minimise the possibility of nerve damage when removing your wisdom tooth, and they should tell you about the risk of complications before the procedure.
GENERAL ANAESTHETIC
General anaesthetic is occasionally needed for the removal of wisdom teeth. It carries some additional risks, but complications are very rare, occurring in less than 1 in every 10,000 cases.