OVERVIEW
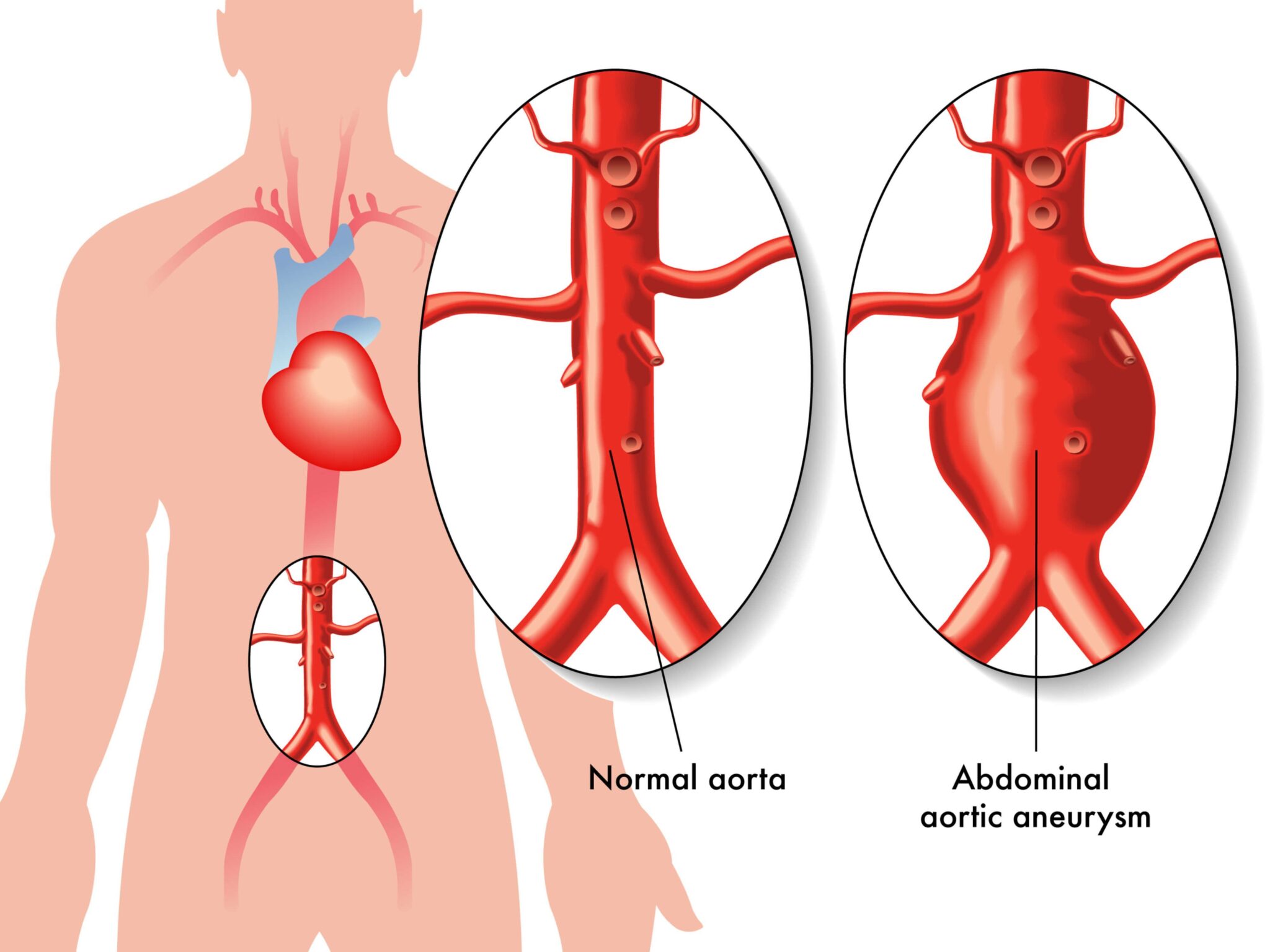
ABDOMINAL AORTIC ANEURYSM (AAA) SCREENING IS A WAY OF CHECKING IF THERE’S A BULGE OR SWELLING IN THE AORTA, THE MAIN BLOOD VESSEL THAT RUNS FROM YOUR HEART DOWN THROUGH YOUR TUMMY.
This bulge or swelling is called an abdominal aortic aneurysm, or AAA.
It can be serious if it’s not spotted early on because it could get bigger and eventually burst (rupture).
WHO’S SCREENED FOR AAA
In England, screening for AAA is offered to men during the year they turn 65.
Men aged 65 or over are most at risk of getting AAAs. Screening can help spot a swelling in the aorta early on when it can usually be treated.
Screening for AAA is not routinely offered to:
- women
- men under 65
- people who have already been treated for an AAA
This is because the risk of getting an AAA is much smaller in these groups.
If you’re over 65 years old, you can ask for a scan to check for an AAA if you think you might need one but have not been offered a screening test.
HOW TO GET SCREENED FOR AAA
If you’re a man and registered with a GP, you’ll get a screening invitation in the post when you’re 64 or soon after your 65th birthday. You can then arrange an appointment that suits you.
If you’re a man over 65 and have not been screened before, you can ask for a test by contacting your local AAA screening service directly.
BENEFITS OF AAA SCREENING
An AAA will often cause few or no obvious symptoms, but if it’s left to get bigger, it could burst and cause life-threatening bleeding inside your tummy.
About 8 in every 10 people who have a burst AAA die before they get to hospital or do not survive emergency surgery to repair it.
Screening can pick up an AAA before it bursts. If an AAA is found, you can choose to have regular scans to monitor it or surgery to stop it bursting.
The screening test is very quick, painless and reliable. Research suggests it can halve the risk of dying from an AAA.
DECIDING TO BE SCREENED
It’s up to you to decide if you want to be screened for AAA. While there are clear benefits of screening, you should also consider the possible risks.
There’s no risk from the screening test itself, but there’s a risk of:
- anxiety from being told you have a potentially life-threatening condition
- serious complications of surgery carried out to treat an AAA
Call your local screening service and ask to be removed from its list if you do not want to be screened.
WHAT HAPPENS DURING AAA SCREENING
Screening for AAA involves a quick and painless ultrasound scan of your tummy. This is similar to the scan pregnant women have to check on their baby. When you arrive for your appointment, a screening technician will check your details, explain the scan and ask if you have any questions.
For the scan:
- you lie down on a table and lift up or unbutton your top (you do not need to undress)
- the gel is wiped away and you pull down or button up your top
- the technician tells you the result straight away
The whole test usually takes about 10 to 15 minutes. Sometimes the technician might not be able to see your aorta clearly. This is not anything to worry about. If this happens, you’ll be asked to have another scan, usually on a different day.
RESULTS OF AAA SCREENING
You’ll be told your result at the end of the test. If a problem is found, you’ll also be a sent letter confirming the result and letting you know what happens next. There are 4 possible screening results.
NO ANEURYSM FOUND
f your aorta is less than 3cm wide, this means it’s not enlarged. Most men have this result. You will not need to have any treatment or monitoring afterwards, and will not be invited for AAA screening again.
SMALL AAA
If you have a small AAA, this means your aorta measures 3cm to 4.4cm across. Just over 1% of men screened have a small AAA. You will not need any treatment at this stage as the chance of the AAA bursting is small. You’ll be invited back for a scan every year to check its size. Treatment will usually only be needed if it becomes a large AAA. You’ll also be given advice on how you can stop an AAA getting bigger, such as stopping smoking, eating healthily and exercising regularly.
MEDIUM AAA
If you have a medium AAA, this means your aorta measures 4.5cm to 5.4cm across. About 0.5% of men screened have a medium AAA. You will not need any treatment at this stage as the chance of the AAA bursting is small. You’ll be invited back for a scan every 3 months to check its size. Treatment will usually only be needed if it becomes a large AAA. You’ll also be given advice on how you can stop an AAA getting bigger, such as stopping smoking, eating healthily and exercising regularly.
LARGE AAA
f you have a large AAA, this means your aorta measures 5.5cm or more across. About 0.1% of men screened have a large AAA. As large AAAs have the highest risk of bursting if left untreated, you’ll be referred to a specialist surgeon within 2 weeks to talk about your treatment options. Most men with a large AAA are advised to have surgery to stop it getting bigger or bursting. While surgery carries a risk of serious complications, this is generally smaller than the risk of not treating a large AAA.
FAQS
IS AAA SCREENING OFFERED OUTSIDE ENGLAND?
AAA screening programmes have been set up in Northern Ireland, Scotland and Wales.
For more information, see:
- Northern Ireland: NI Direct AAA screening
- Scotland: NHS Inform AAA screening
- Wales: NHS Wales AAA Screening Programme
WHAT HAPPENS IF I’M A MAN OVER 65 AND HAVEN’T BEEN SCREENED?
If you’re a man over 65 and you haven’t been screened before, you can contact your local screening service to ask for a scan without going through your GP.
CAN I OPT OUT OF THE SCREENING PROCESS?
You may decide, after you have been invited or have attended screening, that you do not want the NHS AAA Screening Programme to contact you again or provide any ongoing care – either directly, or via any other healthcare professional.
If you ask to be removed from the screening invitation or recall process you will be given information about the risks of your decision. Requests for removal must be made to your local screening unit. If you change your mind, you can ask to be invited for screening again at any time.
WHAT HAPPENS IF I GIVE PERMISSION TO BE CONTACTED ABOUT RESEARCH IN THE NHS AAA SCREENING PROGRAMME?
The NHS AAA Screening Programme works closely with medical researchers to improve screening and the care of men being screened for AAA and men with AAAs. If you give permission for the programme to contact you about research you may be sent information about ongoing research and how to get involved. All involvement in research in the NHS is entirely optional. The decision to take part or not does not affect the care you receive from the NHS. You can decide whether to participate on a project-by-project basis. The programme does not pass any personal information on to medical researchers directly. All research projects must first be approved by the NHS AAA Screening Programme Research Committee.
DOES THE PROGRAMME DO ANYTHING ELSE WITH THE PERSONAL INFORMATION IT KEEPS?
The programme has an obligation to monitor its own performance and determine if it can be improved. This ensures the service is of good quality and achieving its main aim of preventing men dying from the complications of having an aneurysm.
One of the ways the programme measures performance is by monitoring what happens to men who have been invited for screening. It does this by obtaining information for men invited for screening. This information is either held by NHS Digital directly (data on hospital admissions, which is collected from all NHS hospitals) or obtained from other government organisations (data on deaths are held by the Office for National Statistics).
In order to ensure confidentiality, the programme anonymises the data by removing information such as names and dates of birth. It passes on to NHS Digital only men’s NHS numbers, which it uses to link to health records. NHS Digital matches the information provided with the information it holds and, again, removes all identifiable information including NHS numbers.
Anonymous data from the programme and NHS Digital is then passed to the University of Leicester, the programme’s current academic partner. The University of Leicester analyses this information and provides the programme with a report on its performance. At no point will an individual man’s identity be known to the analysis team at the University of Leicester. All data is held securely at the University of Leicester and is not made available to any other parties at any time.
The data resulting from this process will be held for a maximum of 20 years. This is because aneurysms develop very slowly and it takes a long time to properly assess the full benefits of the screening programme.
If you do not want your anonymised healthcare data used in this way then please contact your local screening programme.
COULD I FIND OUT ABOUT OTHER HEALTH PROBLEMS AS A RESULT OF AAA SCREENING?
No. During the screening scan the technician only looks at your aorta to check if you have an AAA. They don’t check for any other health conditions.
If you have any concerns about your health, speak to your GP.
CAN WOMEN AND MEN UNDER 65 BE SCREENED?
AAA screening isn’t routinely offered to women and men under 65 because most burst AAAs occur in men over 65. Men are six times more likely to have an AAA than women.
There’s not enough evidence to suggest that screening women and younger men would deliver major benefits.
But if you think you might be at an increased risk of AAA – for example, because a close family member has had one – talk to your GP about the possibility of having a scan to check for an AAA.
If your GP feels you might benefit from having a scan, this will usually be done when you’re five years younger than the age at which your relative was found to have an AAA.
If you have a family history of AAA, you should take the usual health precautions of not smoking, eating healthily, and exercising regularly. Read more about how to reduce your risk of an AAA.
CAN I DRIVE IF I HAVE AN AAA?
You may need to tell the Driver and Vehicle Licensing Agency (DVLA) if you have an AAA. You may need to stop driving if it’s large.
The DVLA say:
- car and motorcycle drivers must tell the DVLA if their AAA measures more than 6cm and stop driving if it reaches 6.5cm
- bus, coach and lorry drivers must tell the DVLA if they have an AAA of any size and stop driving if it reaches 5.5cm
You can usually drive again once your AAA has been treated. The GOV.UK website has more on how to tell the DVLA about an AAA.
Ask your GP if you’re not sure if you need to inform the DVLA about your AAA or temporarily stop driving.
Having an AAA shouldn’t affect your car insurance premium.
CAN I FLY IF I HAVE AN AAA?
It’s safe to travel by plane if you have an AAA. They’re no more likely to burst at a high altitude than on the ground.
The Association of British Insurers (ABI) has been advised of this and it’s not aware of any airlines that refuse people with an AAA.
CAN I GET TRAVEL INSURANCE IF I HAVE AN AAA?
The ABI is unaware of any travel insurance policies that specifically exclude AAAs as part of their standard wording.
They suggest that anyone with an AAA should declare it during the application process (or when it’s diagnosed, if you already have a travel insurance policy).
If you declare an AAA, you may be asked if you:
- have had surgery (and if so, when you had it)
- are on a waiting list for surgery
- have any other related health conditions You may be charged an additional premium or have the condition excluded from your cover.
When looking for cover, a broker can help. The British Insurance Brokers Association (BIBA) operates a find a broker service that can help – they can be contacted on 0370 950 1790.
WHAT PERMISSION DO I NEED TO GIVE TO BE SCREENED?
At the screening clinic, you’ll be asked to give permission:
- for the programme to store information about you and your visit on the national AAA screening IT system, and to use this information to help offer safe and effective screening
- for the programme to screen you for an AAA (which involves a scan of your tummy) and to tell you the result
- if you’re found to have an AAA, to share your personal information with a vascular surgeon through the National Vascular Registry You’ll only be screened if you give consent to all three points.
You’ll also be asked if the screening programme can use your information to contact you in the future about research that’s going on in the programme. You don’t have to give permission for this to be screened.
WHY DO I NEED TO GIVE PERMISSION FOR THE PROGRAMME TO KEEP MY PERSONAL INFORMATION IF I WANT TO BE SCREENED?
Screening is a diagnostic procedure that requires the person’s consent.
WHY DOES MY DATA NEED TO BE RECORDED?
There is a duty of care to record what has been done and what has been found during screening and to share this with appropriate healthcare providers, so any findings can be followed up.
Recording data enables the programme to ensure that you are screened, assessed and treated in an effective and timely way.
The abdominal scan is only one part of a systematic pathway of care. It would be irresponsible and potentially negligent to offer a scan without ensuring that the safeguards offered by an assured national system are in place.
The screening programme needs to retain personal data so it knows if and when a man has been scanned and if he has declined screening.
Recording data also enables local programmes to keep track of who has been invited for screening and deal with follow-up enquiries.
HOW IS MY PERSONAL INFORMATION STORED?
The programme controls and processes personal information for the purposes of providing the screening service in a way that is compatible with the Data Protection Act (the data controller). The programme uses a third party (Northgate Public Services) to process and manage this personal information in a secure database.
Although the database is a national system, strict data governance means your personal details can only be accessed by healthcare professionals involved directly in your screening or any subsequent assessment or treatment.
If you are screened and found to have an aneurysm, this information will need to be shared with a vascular unit so you can get further tests and potentially surgery.